News All News
June 22nd, 2023
Turning Cancer on Itself
New thinking about cancer could lead to a paradigm shift in the way doctors treat the disease
By Steve Neumann

President Richard Nixon declared war on cancer in 1971. At the time, the disease was the second leading cause of death in the US.
More than 50 years later, cancer is still the country’s second most lethal disease, claiming over 600,000 lives every year. Despite advances in treatment—chemotherapy, for instance, is less torturous than it was decades ago—there is still no cure.
GSAS student Liang Chang hopes to change that.
“[My research] is in a super early stage, and making a drug is financially risky for pharma companies,” Chang says, “but I really believe that this work could be an opportunity for a new class of cancer medicine in the future.”
As a PhD student in biological and biomedical sciences, Chang is pioneering a new approach to cancer treatment, one that targets the genes required for the disease’s growth and survival. If he’s successful, his research could effect a paradigm shift in the treatment of some types of cancer—saving countless lives in the process.
Targeted Impact
The vast majority of therapeutics are organized around the idea that cancers need something to keep them growing. That’s why most are aimed at blocking or deleting genes and signaling pathways—those biochemical processes that control functions like cell division or death.
The problem with this approach is that it kills normal healthy cells as well as cancerous ones. That’s why patients sometimes experience side effects like hair loss, bruising and bleeding, and gastrointestinal distress from chemotherapies. There are some targeted inhibitor drugs that aim to block signaling more specifically in cancer cells, but only a small fraction of patients with the “right genetic mutations” can benefit from them.
Chang’s research, on the other hand, focuses on turning on aspects of the signaling pathways that will be selectively lethal in cancer cells, not healthy ones.
Part of the inspiration for this counter-intuitive approach can be seen in the mechanism of action for an FDA-approved drug known as a BRAF inhibitor. The BRAF gene belongs to a class known as oncogenes that, when mutated, have the potential to cause normal cells to become cancerous. The drug selectively targets BRAF, interfering with the mitogen-activated protein kinase (MAPK) signaling pathway that regulates the proliferation and survival of melanoma cells.
When you treat the melanoma with the inhibitor, the tumor starts shrinking—until it develops resistance and starts to grow again. When the drug is withdrawn, however, the tumor starts shrinking once more. Unfortunately, it figures out a way to adapt to that, too, and starts growing yet again.
But the fact that the tumor started to shrink when the gene inhibitor was taken away is what made Chang speculate that activating the MAPK signaling pathway might lead to a viable therapeutic approach to selectively killing cancer cells.
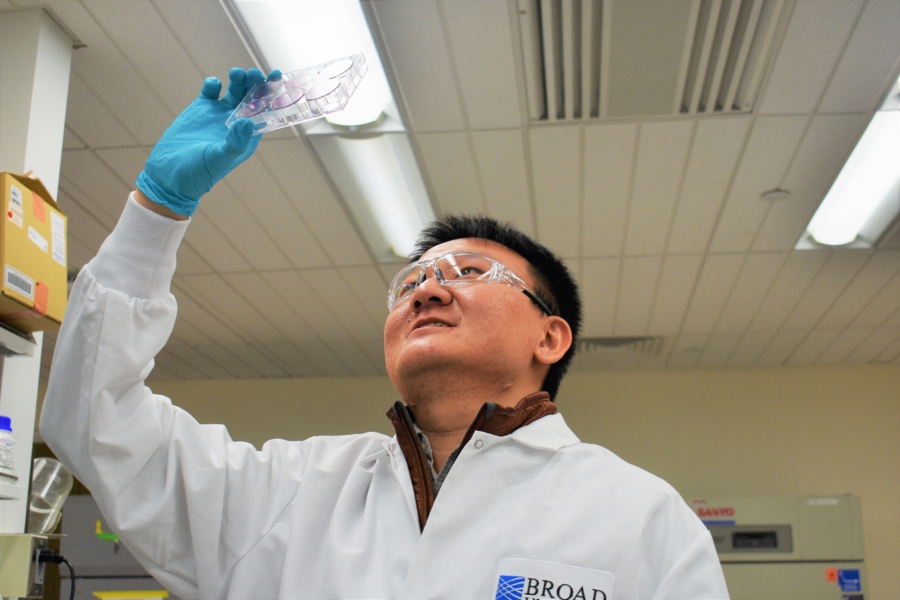
Liang Chang is a PhD student in biological and biomedical sciences.
“The concept is that, if a cancer cell gene already has a mutation or alteration that turns on a specific signaling pathway, then it is actually vulnerable to further turning on the pathway,” Chang says. “And I found that if we further turn on the pathway, only the cancer cell that already has the pathway turned on dies first.”
In all, Chang has been able to turn on 10 signaling pathway nodes in 500 cancer cell lines at the same time, through a novel method he spent months developing. He has validated these findings in cancer patient-derived tumors kept viable in Petri dishes, as well as in a mouse tumor xenograft—basically, a human tumor grown in a mouse.
“What we found was that across all of these models, turning on the one pathway selectively kills the cancers that already have a mutation that turns on that pathway, but not the cancer cells that don't,” Chang says.
What we found was that . . . turning on the one [signaling] pathway selectively kills the cancers that already have a mutation that turns on that pathway, but not the cancer cells that don't.
—Liang Chang
This work has enabled him to create the Cancer Dependency Map, an initiative started by the Broad Institute, where Chang conducts his research in collaboration with other academic institutions and industry partners. Its purpose is to represent a landscape of genetic targets for therapeutic development, identify patients who respond to these therapies, and develop a better understanding of the vulnerabilities of cancer.
Proof of Concept
Chang’s dissertation supervisor, William Sellers, a Harvard Medical School (HMS) professor and the director of the cancer program at the Broad Institute, says that his advisee’s approach has enormous implications for the way scientists think about cancer research. “If it turns out cancers are equally susceptible to turning things on,” says Sellers, “it means we kind of missed an entire area, or even thought process, of how to make new cancer therapeutics.”
HMS professor Kornelia Polyak, who is on Chang’s dissertation committee, also believes the student’s targeted methodology might be a viable therapeutic approach in certain tumor types such as melanoma, colorectal, and endometrial cancer.
“Traditionally, most therapeutic targets are evaluated by deleting genes or blocking signaling pathways, but Liang did the opposite: he overactivated them,” Polyak says. “Systemic overactivation of oncogenic pathways is not likely to be a feasible therapeutic approach since it can cause cancer; that’s why cancer cell-specific delivery is likely to be essential.”
Sellers notes that the principal impediment to curative therapeutics for cancer to date has been the emergence of drug resistance. However, if Chang’s approach were to be used in tandem with traditional chemotherapy, resistance might no longer be an insurmountable problem.
“What's interesting [in Chang’s work] is this idea that if you could impair the growth of cancer either by turning something off or turning something on, the odds that the cancer cell could generate resistance mechanisms to both of those types of events at the same time would be relatively rare,” Sellers says.
. . . if you could impair the growth of cancer either by turning something off or turning something on, the odds that the cancer cell could generate resistance mechanisms to both of those types of events at the same time would be relatively rare.
—Professor William Sellers
Sellers is confident in the validity of his advisee’s results, not just because of Chang’s technical prowess, but also because of the assiduousness of his methodology.
“Liang took a lot of time and care in optimizing the experimental approach, down to a lot of different very important details,” he says. “Then once it was optimized, and the data generation part happened, the quality of the data was simply outstanding.”
Chang believes his research could lead to robust anti-tumor effects in cancer patients.
“Our work provides an important proof of concept that this conditional pathway activation is a more common selective cancer vulnerability than previously appreciated and highlights new therapeutic opportunities in diverse sets of cancers,” he says, “because more than 70 percent of all cancer patients have a mutation in one of these pathways.”
From China, with Love
A first-generation college student from China, Chang credits his academic success to the love and support of his father, a police officer, and mother, a retired accountant. “They really appreciate education and science in particular, and they always felt like a college education was something I should get,” he says.
Because of his parent’s encouragement, Chang had a passion for both medicine and politics growing up. When he first enrolled at Macalester College in 2012 as an undergrad, Chang was on a pre-med track but wanted to try his hand at politics first.
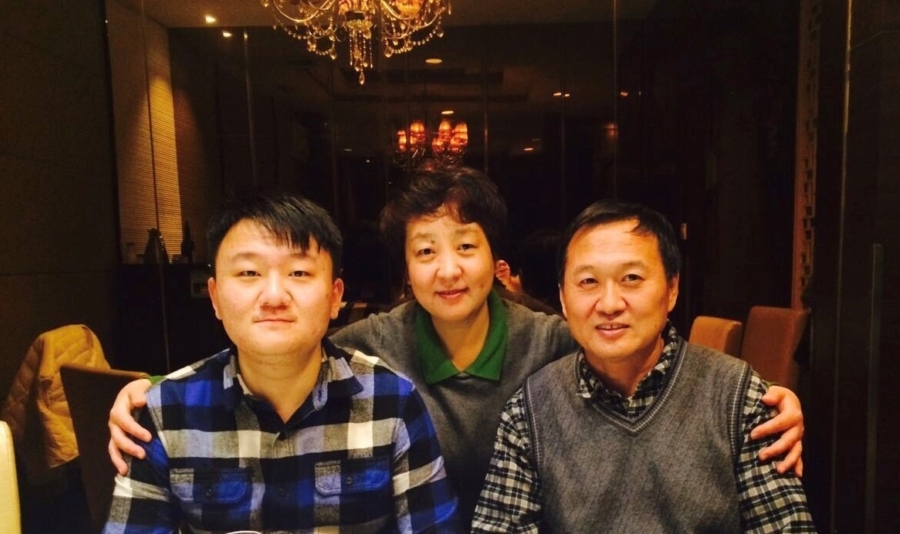
Liang Chang (left) with his parents.
“Politics is all about allocating resources to make change,” Chang says. “But one semester in, I felt like politics was more about talking about problems, which was far away from making a real impact. I began to think that biomedical research was the way because I can use my own hands to effect real change.”
In the long term, Chang wants to pivot away from the research lab to the corporate office, so he can learn how to bridge the gap between scientific research and the development and marketing of actual medicines.
“I feel like my research can potentially make someone in the big pharmaceutical companies get interested in this,” Chang says, “but I also feel like, to make the ultimate impact—to make something into a drug—I need to leverage the business side.”
In addition to his cancer research, Chang has worked for two years as a senior business development fellow at Harvard’s Office of Technology Development. There, he assesses new technologies produced at Harvard Labs and thinks about how to convert them either into new companies or license them to existing firms.
“I actually have started a company that's backed by Google Ventures,” Sellers says, “so there will be at least one company working on my approach to cancer therapeutics.”
Sellers adds that his group also has a grant of $500,000 from pharmaceutical-giant Novartis to profile even more genes and pathways across the 500 cell lines they have, using the method established by Chang. With this support—and that of his Harvard advisors and mentors—the GSAS student is on track to reach his ultimate goal—having a positive impact on society.
Photos courtesy Liang Chang
Tags: Gazette
Press Contact: Kirsten Mabry | (617) 495-4157
